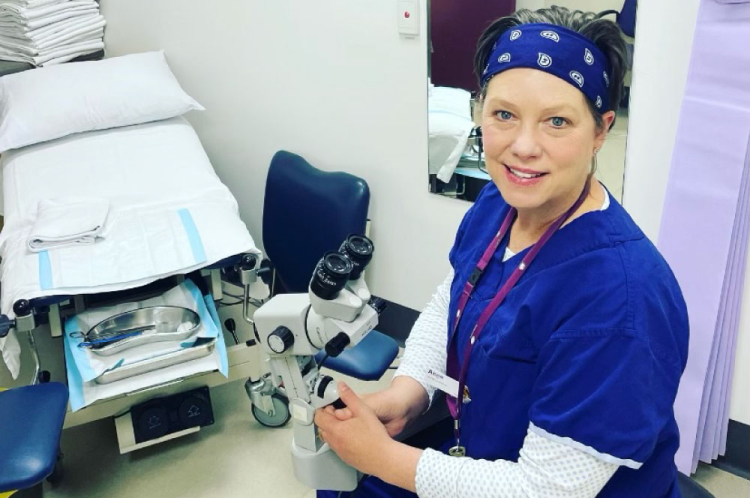
The Royal Women’s Hospital nurse Ange Steele is on the frontline in the fight to eliminate cervical cancer. She shared her story ahead of International Gynaecological Awareness Day (10 September) and Gynaecological Cancer Awareness Month.
Ange Steele is the Nurse Coordinator of the Women’s Dysplasia Clinic and Director of the Board of the Australian Centre for the Prevention of Cervical Cancer. She is also the first nurse in Victoria to be trained in colposcopy, an examination of the cervix that occurs after a positive or abnormal cervical screening test. A colposcopy allows specialists to find any changes to the cells in the cervix which can lead to cervical cancer, and to assess the extent of the changes.
Traditionally, only surgeons and gynaecologists have been able to perform a colposcopy. It is only in recent years – and mostly in the UK and New Zealand – that nurses have been trained to perform the potentially life-saving procedure. Now nurse colposcopy clinics are set to be one of the key drivers in the race to eliminate cervical cancer, and Ange is leading the way.
A passion to provide greater access to screening
Modelling published in the Lancet in 2019 suggests that Australia is on track to eliminate cervical cancer as a public health problem by 2030. The three pillars that are helping to drive elimination in Australia are vaccination, cervical screening and treatment. A colposcopy is part of the screening process and a critical aspect in the elimination of cervical cancer.
Data from the Australian Centre for the Prevention of Cervical Cancer shows that people most at risk of developing cervical cancer include those in the Aboriginal and Torres Strait Islander and LGBTIQ+ communities, homeless women, and people in rural and remote communities.
Ange says that nurse colposcopy clinics are an important way to reach these communities and continue to drive down the rate of cervical cancer in Australia. Having worked in the UK where nurse-led colposcopy clinics were common, Ange wanted the same screening opportunities for women in Australia.
“To see women present to hospital with invasive cervical cancer is devastating for us as health professionals because we know that cervical cancer is preventable,” she says.
“Nurses are more mobile than gynaecologists and surgeons, who are tied to bigger tertiary hospitals and do more complicated work. Nurses can help to ease demand for colposcopy clinics in our hospitals, as well as reach those women in rural and remote areas that find access to screening and services much more difficult.”
Making a difference in the fight against cervical cancer
Ange’s journey to cervical cancer screening advocate began in 1991 when she joined the Women’s as a midwife. Later, Ange trained as a cervical cancer screening nurse and then made her way into the Women’s Gynaeoncology Service and the Dysplasia Clinic.
She has been a nurse in cervical screening for 22 years and saw colposcopy as the next step in her career. With the encouragement and support of her manager, the Women’s gynaecology specialist David Wrede, Ange completed colposcopy training in 2021. She is currently performing colposcopies under the supervision of senior clinicians in the Women’s Dysplasia Clinic while she works towards accreditation.
Ange says the support and foresight of her colleagues has been instrumental to her undertaking colposcopy training and extending her practice as a nurse.
“I can’t tell you how much I love this work,” Ange says. “One of the nicest things to have come out of it is the amazing collaboration between myself and the doctors in the team – I feel like they’re cheering me on from the sidelines.”
As a nurse representative on the Australian Cancer Prevention Board, Ange is helping to inform government about building a curriculum and training program for nurses and establish nurse colposcopy clinics throughout Australia.
“It’s a really a terrific opportunity,” she says. “Being a part of the fight against cervical cancer makes me excited to come to work every day, because I know I am making a difference.”