
So, you are now around 20 to 21 weeks of your pregnancy!
From now until you give birth, we will regularly send you new information about pregnancy. If you don't want to receive this information, please call (03) 8345 3272 or email patientexperience@thewomens.org.au
Part 1. This stage of your pregnancy

We’ll schedule routine pregnancy appointments around the following weeks of your pregnancy:
- Week 22
- Week 28
- Week 32
- Week 34
- Week 36
- Week 38
- Week 40
At each appointment a midwife or doctor will:
- follow up and discuss any tests you’ve had or will be having
- check your physical health, for example, your blood pressure
- answer any questions you have (it’s helpful to write these down before your visit)
- check your baby’s growth. As your baby grows, they’ll also check your baby’s position by feeling and measuring the size of your belly and listening to your baby’s heartbeat.
Before your first appointment, you’ll need to complete a series of blood tests to check for:
- your blood group and iron levels
- immunity to rubella (German measles)
- exposure to hepatitis (a liver disease)
- sexually transmitted diseases such as syphilis and HIV - this test includes counselling before and after the test
- thalassaemia, an inherited condition affecting the protein (haemoglobin) in blood that carries oxygen around your body and to your baby
- vitamin D deficiency and hepatitis C – for those at risk.

We also ask about:
- whether you have support from family and friends
- any past miscarriages or abortions
- family violence (for more information visit the Pregnancy, Birth and Baby website

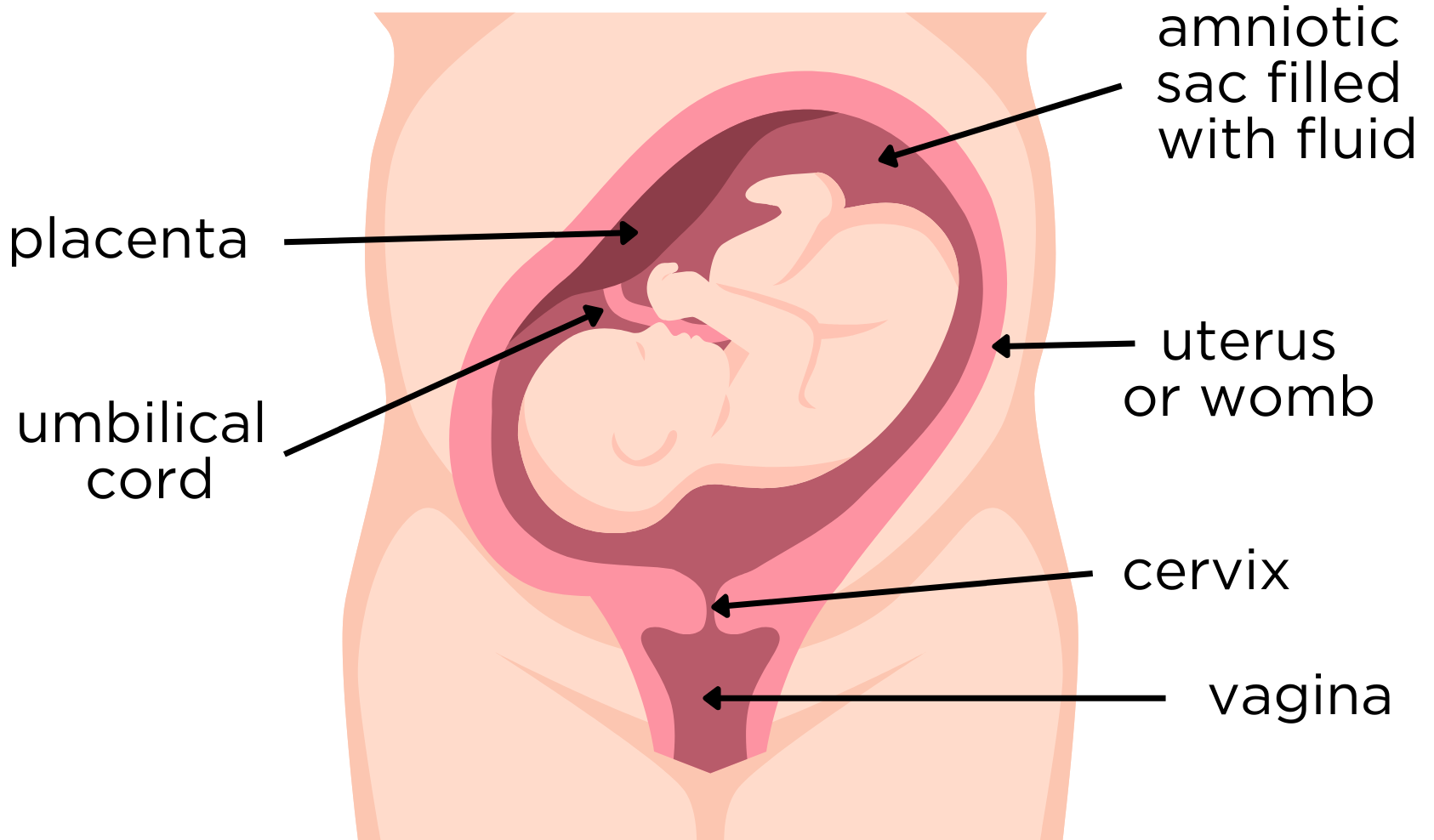
Throughout your pregnancy, you’ll hear a lot about different parts of your body. Some words may be new to you. Here are some you’ll hear often:
Amniotic fluid - this is often called your waters. It’s contained in the bag (amniotic sac) that surrounds your baby during pregnancy. The amount of fluid varies throughout your pregnancy.
The fluid has several important functions.
- It maintains a consistent temperature in the uterus (womb) for your baby.
- It provides protection from minor bumps.
- It flows in and out of your baby’s lungs. At around 36 weeks, the placenta produces a hormone that helps your baby’s lungs mature so they can breathe oxygen after birth.
- Your baby swallows the fluid which helps develop their taste buds. The swallowed fluid can pass through their kidneys and contribute to fresh amniotic fluid. Or it may be stored in the baby’s bowels and later passed as meconium, a sticky, thick, dark green poo after birth.
- In a healthy pregnancy, the fluid is constantly replaced by the baby’s urine and the placenta.
Usually, the amniotic sac breaks shortly before or during labour. Occasionally, it may break weeks before your due date.
Contact the hospital immediately if you think your waters have broken. Ring (03) 8345 3635.
Antenatal - refers to the time during pregnancy up until birth.
Cervix - the neck or entrance to your uterus. It’s a long, thick tube that is usually closed. As you get closer to your due date and during contractions, your cervix becomes softer, shorter, and starts to open.
During pregnancy, a thick mucous develops in the cervix. This mucous is very sticky and contains lots of antibodies. It forms a mucous plug that blocks the cervix, helping prevent infections from entering your uterus. It comes out of your vagina as the cervix starts to open, sometimes before labour begins or during early labour. This is called a show.
Conception - (or fertilisation) happens when a sperm joins with an egg, starting a pregnancy.
Endometrium - the lining of the uterus. After your baby and placenta have been birthed, the endometrium will also come out of your body. This lining, along with bleeding from the placenta site, will cause bleeding from your vagina for about 7 to 14 days, sometimes longer.
Fundus – this is the upper edge of the uterus. As your baby grows, the uterus gets bigger, and the fundus rises. During a clinic visit, your doctor or midwife will measure the distance between your pubic bone (symphysis pubis) and the fundus.
Gestation - the time when a baby grows inside your uterus before birth.
Perinatal - this is the time during pregnancy and the first year after birth.
Placenta – also called the afterbirth. It forms soon after conception and attaches to the wall of the uterus and connects to your baby via the umbilical cord. It’s responsible for the growth of your baby. It’s well established by the 10th day of pregnancy, with good blood flow through the umbilical cord by the 10th week of pregnancy.
The placenta supplies your baby with nutrients and oxygen, removes waste, and acts as a barrier against some substances. However, harmful substances like alcohol, nicotine, and other drugs can travel through your blood, into the placenta, and then to your baby.
The placenta also produces hormones to help support your pregnancy.
After your baby is born, you will birth the placenta. This is why it’s often called the afterbirth.
The placenta’s position depends on where its cells attach to the uterus wall. Usually, it attaches higher up in the uterus. But sometimes it attaches lower down, near or over the cervix. This is called placenta praevia. This can cause complications, including bleeding. In these cases, a caesarean birth may be necessary.
However, when the placenta is low early in pregnancy, it will usually grow upwards, away from the cervix as the uterus gets bigger.
Postnatal - refers to the time after birth, usually lasting for 6 to 8 weeks.
Uterus - commonly called the womb (pronounced woom), the uterus is a muscular organ, shaped like an upside-down pear.
Learn more
For more pregnancy and labour definitions, visit the Pregnancy, Birth and Baby website glossary.

When you have a blood test, it will show your blood type. These tests also tell us if you have Rh positive or Rh negative blood. Most people are Rh positive.
If you are Rh negative and your baby is Rh positive, it may cause health problems during pregnancy. These can be treated with Anti-D injections at 28 and 34 weeks.
You’ll learn more about Anti-D in week 27.

You can find your test results through Health Hub, or you’ll receive them at an appointment where you can discuss them.
Test results can’t be given over the phone.
If your midwife or doctor has any concerns about your results, they’ll contact you by letter or phone.

At your first hospital visit, your midwife or doctor will help you work out your baby’s estimated due date.
The average length of pregnancy (or gestation) is counted as 40 weeks. The start of a pregnancy is counted from the first day of your last period, not the date of conception, which usually occurs 2 weeks later.
So, a baby is considered:
- early term if it’s born between 37 weeks and 38 weeks, 6 days
- full term if it's born between 39 weeks and 40 weeks, 6 days
- late term if it’s born between 41 weeks and 41 weeks, 6 days.
We estimate your baby’s birth date by looking at:
- the date of your last normal menstrual period (LNMP)
- the pattern of your menstrual cycles, including how long they usually last, and how often they occur
- any contraception used before you got pregnant.
We also use a dating ultrasound or a dating scan to estimate your baby’s due date. This scan happens between 8 and 14 weeks, usually before 12 weeks.
If you have a regular menstrual cycle, an early ultrasound usually gives a similar estimate of your baby’s age and due date as your last normal period. When the dates are close (within a few days of each other), either can be used for the due date. But if they’re more the 5 days apart, the ultrasound due date is more reliable, and your due date may be changed at your first hospital visit.

During pregnancy, ultrasound scans are done to create a picture of your baby, your uterus, your cervix, and your pelvis. You may have an ultrasound several times during pregnancy to check how your baby is developing, if needed.
The ultrasound uses sound waves. This is safe for both you and your baby. It is different to an x-ray.
Your 18 to 20-week ultrasound scan is also known as the morphology scan or fetal anomaly scan. It looks for abnormalities in your baby's structural development and growth. It also checks the position of the placenta and the length of your cervix. This scan gives you the chance to see your baby, often for the first time.
A morphology scan is a routine antenatal test and is very important because it checks:
- how many babies there are
- where the placenta and the umbilical cord are positioned
- the amount of fluid around your baby
- that your cervix is closed
- your baby’s growth, including the head, belly, and long bones of the arms and legs
- any structural abnormalities or problems in the baby’s spine, brain, heart, stomach or lungs.
You can have the scan over your belly (transabdominal) or through your vagina (transvaginal). The preferred method is transvaginal as it allows the person doing the scan (sonographer) to accurately assess the length of your cervix and get better pictures.
During the ultrasound, a thin probe is inserted into your vagina. It’s a safe procedure that most people don’t find uncomfortable.

Abnormality with your baby
If the ultrasound finds something unusual with your baby, it means there might be an abnormality. Most babies are usually fine, but about 2 to 3 out of every 100 pregnancies (2-3%) will have an abnormality. Many major abnormalities can be seen at the 18 to 20-week ultrasound, but not all problems can be found this way.
Conditions like cerebral palsy, autism, or some heart defects may not show up on ultrasound. Sometimes, a problem might be small or hard to see or is caused by something not visible in a scan of the baby’s organs.
If an abnormality is found, a maternal fetal medicine specialist will talk with you about what it could mean. They may recommend further tests to confirm the diagnosis and discuss available treatment options. Whatever you decide to do, we’re here to provide ongoing counselling and support.
Abnormality with your placenta
During a morphology scan, we record the position of the placenta. If it’s near the cervix. the distance is measured. Another scan may be recommended between 32 and 34 weeks to make sure the placenta has moved away from the cervix. By this time, most placentas have moved.
Abnormality with your cervix
During the scan, we measure the length of your cervix. A shorter cervix might increase the chance of your baby being born preterm (before 37 weeks).
If you have a short cervix, there are several options available. Your doctor or midwife will discuss these with you if necessary. They will also refer you to the Women’s specialist Preterm Labour Clinic. It provides specialist care for people at risk of preterm delivery.
Part 2. Things to consider
Childbirth education
We offer our childbirth education information in several ways:

We provide group childbirth education programs for first-time parents giving birth at the Women's.
These programs are available in person at Parkville or online. Sessions run on weekends, weekdays, and evenings.
We also have special programs for families expecting twins (or more!), LGBTQIA+ /Rainbow parents, and some programs are available in languages other than English.
Each program has 2 or 3 sessions, depending on the program. We also offer 1-day intensive programs. Sessions last between 1.5 to 6 hours, with most running 3 to 4 hours.
Aim to choose a program that starts when you’re around 28 to 32 weeks pregnant. Your partner or support person is welcome to come with you.
Book your spot as soon as possible so you don’t miss out. Classes fill up fast, and early booking gives you more options.
Bookings are made online, via Eventbrite. To go straight to available dates and booking, visit the Eventbrite booking page.
Benefits of childbirth education
- Gain confidence in your pregnancy, labour, birth, breastfeeding, and the early weeks of parenting.
- Learn about care options to make informed choices.
- Involve your partner or support person in the parenting journey.
What you’ll learn
All group classes are designed to provide participants (and their support persons) with the knowledge to navigate late pregnancy, labour, birth, breastfeeding, and early parenthood.
An experienced midwife will cover topics such as:
- signs of labour and when to go to the hospital
- how labour and birth progress
- supporting someone in labour
- practical coping methods during labour
- medical options for pain management
- medical assistance for birth
- understanding breastfeeding
- safe sleeping and settling for your baby
- communicating with your baby
- community support services for the family.
Cost
- Classes are free for public patients giving birth at the Women’s (no payment required).
- Private patients booked at the Women’s and people without a Medicare card must pay a fee at checkout. This fee covers the entire course and is refundable if you cancel at least 1 week before the first class. Program fees range from $250 to $450. For more details, visit Eventbrite.
- Some private health funds may provide a rebate for the program. To find out more, check with your health fund. Each ticket covers 1 pregnant person and 1 support person (2 people total).
How to book
You can view available dates and secure your place on the Eventbrite booking page.
Booking tips
- Plan to attend classes at around 28 to 34 weeks of your pregnancy.
- Book early - places are limited.
- Register for only 1 program (extra bookings will be cancelled).
- New programs are added at the start of each month.
- There is no waitlist - check the Eventbrite website regularly for cancellations.
- Use the pregnant person’s name when booking.
- Provide the pregnant person’s hospital Medical Record Number and Medicare card number when booking.
Eventbrite will send a confirmation email after booking.
How to cancel or reschedule
- To reschedule, cancel your booking on Eventbrite and book into another course.
- Please cancel your old booking so someone else can take your spot.
- If you miss a class, we can’t offer a “make-up” session. However, you will receive written summaries before the program starts.
For more information
Email: childbirth.ed@thewomens.org.au
Please note, our office operates part-time during business hours. We’ll respond to your enquiry as soon as possible.

This option is available at any time:
- Watch our 10 online videos
- Read our booklet Birth and babies for first-time parents
- Take a virtual tour through the hospital, birth centre and postnatal ward.
- Check out our fact sheets.
We hope you found this information helpful.
If you have any health concerns, please talk to one of your health care professionals including your midwife, General Practitioner (GP) or your hospital doctor, etc.
We’ll be back in touch next week with more to read and learn. Stay safe and well.